Value-Based Purchasing: What Every Hospital Leader Must Know
What Is Value Based Purchasing?
Value-Based Purchasing is a CMS initiative that adjusts Medicare payments to hospitals based on the quality, not just the quantity, of care they deliver. Under the Hospital Value-Based Purchasing (VBP) Program, hospitals can earn back a percentage of their Medicare reimbursement withholding based on performance in four domains:
- Clinical Outcomes
- Patient Experience
- Safety
- Efficiency & Cost Reduction
This means hospitals are no longer just reimbursed for quantity of services rendered; they are rewarded or penalized based on how well they perform compared to peers and against their historical performance.
Under Medicare’s Hospital Value-Based Purchasing (VBP) Program, hospitals receive payment adjustments based on their performance across the aforementioned domains.
Each year, CMS Value-Based Purchasing withholds a percentage of all participating hospitals’ base Medicare payments (currently 2%). That money goes into a pool, which is then redistributed based on performance scores.
- Hospitals that perform well in the VBP domains can earn back more than they contributed, resulting in a bonus.
- Hospitals that under perform may earn back less than they contributed—or nothing—both resulting in a financial penalty.
Here’s the critical piece:
👉 A poor performance in just one domain (e.g., sepsis mortality, sepsis compliance, readmissions, HCAHPS scores, or HACs) can significantly reduce a hospital’s total performance score.
Because CMS calculates an overall Total Performance Score that includes all domains, weak results in even one area can easily drag down the composite score enough to trigger a negative payment adjustment the following fiscal year.
Example:
- A hospital scores well in safety, efficiency, and cost reduction, but under performs on patient experience (HCAHPS).
- The low domain score reduces their Total Performance Score below the threshold.
- As a result, the hospital receives less than their withholding from the VBP pool.
- This shortfall becomes a penalty applied to all Medicare inpatient payments for the next fiscal year.
Figure 1: Visual of Value-Based Purchasing (VBP) Program
| CMS Value-Based Purchasing Steps | Step Description |
| Withhold | CMS withholds 2% of base Medicare payments from all hospitals. |
| Performance Scoring | Hospitals are scored across four domains: 1) Clinical Outcomes, 2) Safety, 3) Patient Experience, 4) Efficiency / Cost Reduction & Equity |
| Redistribution Funds | Funds redistributed from the pool based on each hospital’s Total Performance Score. |
| Bonus or Penalty | Higher performers earn back more than 2% (bonus). Lower performers earn back less than their 2% withholding resulting in a financial penalty for the following financial year. |
| Weak Domain Impact | Poor performance in even one domain lowers the Total Performance Score and can often trigger a penalty. |
As previously mentioned, Medicare’s Hospital Value-Based Purchasing (VBP) Program adjusts hospital payments based on performance in multiple domains. Each year, 2% of base Medicare payments are withheld and redistributed based on Total Performance Scores.
Figure 2: Financial Example - Demonstrates how poor performance in a single Value-Based Purchasing domain can translate into significant financial penalties for hospitals in the following fiscal year.
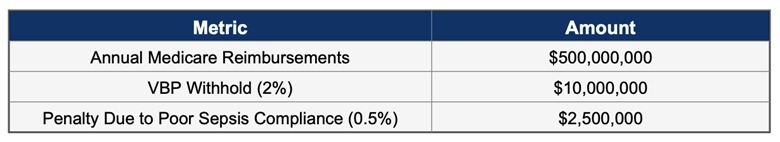
Key Takeaway:
- In this example, Hospital Y’s low sepsis compliance score in the safety domain triggers a 0.5% penalty. This could result in roughly a $2.5M reduction in Medicare reimbursements for the next fiscal year.
- Even one weak domain (like sepsis Sep-1 bundle compliance ) can reduce a hospital’s overall score and trigger penalties across all Medicare payments in the following fiscal year.
- While the actual penalty calculation is much more complex than the example given, the figure demonstrates that considerable money is at risk for hospitals.
Why C-Suite Executives Must Pay Attention
For CFOs, COOs, and CEOs, the VBP program is not just a quality initiative. It is a bottom-line issue. Each year, CMS withholds 2% of Medicare reimbursements across participating hospitals, redistributing that pool based on performance. In the example above, for a mid-sized single hospital, that could mean several million dollars in penalties on the line annually.
But the impact extends beyond immediate financial incentives. VBP performance affects:
- Public reputation via CMS Care Compare scores
- Contract negotiations with payers
- Board-level accountability for financial and operational outcomes
What Domains Matter?
The VBP Program currently evaluates hospitals across these domains:
- Clinical Outcomes (25%) – Measures like mortality for AMI, heart failure, and pneumonia.
- Patient Experience (25%) – Based on HCAHPS survey results.
- Safety (25%) – Tracks Quality Compliance and HACs (e.g., Sepsis SEP-1 compliance, CLABSI, CAUTI).
- Efficiency, Cost Reduction & Equity (25%) – Focuses on Medicare Spending per Beneficiary (MSPB).
Each domain represents operational levers hospital leaders can influence through strategic investments in technology, care coordination, workforce development, or process redesign.
Strategic Questions for the C-Suite
If you're leading a hospital, here are critical questions to bring to your leadership table:
1. Strategic & Financial Alignment
- How is your organization currently performing under CMS’s Value-Based Purchasing (VBP) program?
- Which VBP domains (clinical outcomes, safety, patient experience, efficiency, equity) are creating the most financial pressure?
- Do we know if we are getting penalized for our performances in any of the VBP domains?
- How do you quantify the ROI of your VBP initiatives today?
- What portion of your reimbursements are currently at risk under value-based models?
2. Clinical Outcomes & Quality Measures
- Which quality metrics are the most challenging to meet consistently (e.g., sepsis SEP-1 compliance, readmissions, mortality)?
- Where do you see the biggest gaps between your clinical outcomes and benchmark performance?
- How do you currently monitor performance on SEP-1 care bundle delivery, readmission reduction, or HAC measures in real time?
- How do you ensure consistency in documentation and coding to capture performance accurately?
3. Operational & Workflow Challenges
- What are the biggest barriers your teams face in complying with VBP quality measures?
- How do you identify and address patients at risk of readmission during their first admission?
- How well do your frontline staff feel supported in meeting sepsis bundles or other time-sensitive measures?
- Are there bottlenecks in communication between departments (ED, ICU, floor nursing, case management) that impact VBP performance?
4. Data & Technology Readiness
- How do you leverage EHR data for real-time decision support related to VBP measures?
- Do you feel your current analytics tools provide enough actionable insight to prevent penalties?
- What’s your strategy for integrating data from bedside monitoring, A/V solutions, and EHR to improve VBP scores?
- Are dashboards and notifications being used effectively by clinicians—or are they creating fatigue?
5. Patient & Family Engagement
- How is your organization addressing the patient experience portion of VBP (HCAHPS)?
- What strategies do you have in place to engage patients and families in their care to reduce readmissions?
- Where do you see the biggest gaps in post-discharge follow-up?
6. Strategic Future Readiness
- With CMS expanding equity measures in VBP, how is your organization preparing to address health disparities?
- How confident are you that your current systems will keep pace with upcoming CMS program changes?
- Where do you see the greatest opportunity to improve both clinical outcomes and financial performance simultaneously?
Conclusion
Understanding and optimizing VBP is no longer optional. Many hospitals are losing Medicare reimbursement dollars because of their performance on sepsis and don’t even realize it. It's a strategic necessity to optimize your VBP performance across all domains especially for hospitals navigating tightening margins and increased scrutiny. The good news is that, with the correct data, leadership alignment, and quality improvement strategy, hospitals can not only avoid penalties but also generate meaningful financial upside.
Contact us today to learn how your facility can avoid VBP domain penalties from poor performances, especially in the safety domain around sepsis.

