Remote Patient Monitoring and the Virtual ICU
By Tim Kuebelbeck, Chief Customer Officer at Ambient Clinical Analytics
As we slowly emerge from the COVID pandemic our goal is simple; help doctors, nurses, hospitals, and health systems solve clinical issues using innovative technology and best practices for Remote Patient Monitoring and the Virtual ICU. The pandemic has been a defining event in many ways for remote patient monitoring and virtual ICU’s. There is a shortage of intensivists in the United States, and the demand for them is increasing with our aging population.¹ At Ambient Clinical Analytics we have learned that a virtual ICU and remote patient monitoring with a smart data visualization approach and innovative technology helps save lives and reduces costs. This blog is to help you understand the importance of remote patient monitoring and virtual ICU’s and why every hospital and health system should either be evaluating, deploying, or already utilizing a novel solution.
Virtual ICU intensivists and nurses providing services to multiple care centers, regardless of their location, is an enormous care advantage for hospitals that don’t have any or adequate intensivists or are not located in a major metropolitan area. A virtual ICU, often at an off-site location, connects critical care teams (both intensivists and nurses) with local caregivers, patients, and families for the purpose of caring for patients located in a hospital setting using audio, video, and clinical decision support tools. Remote intensivists and nurses require the same access to patient data as those who are practicing at the bedside. Many of today’s virtual ICU settings have access to excellent audio and visual tools but are lacking the clinical decision support and smart data visualization tools needed to provide the best care possible for ICU patients. One important point to consider as you read this article is that many virtual ICU solutions were designed for critical care only and are not malleable to general inpatient beds.
Using novel remote patient monitoring solutions such as Ambient Clinical Analytics AWARE™ Critical Care, along with audio and visual virtual ICU solutions, provides alerting for issues like sepsis, heart failure, and patient decompensation that increases efficiency and improves clinical outcomes. Disruptive virtual ICU solutions must also monitor other changes in patient status including medication changes, abnormal labs, etc. Any virtual ICU solution you choose must promote situational awareness for patients in all hospital locations, including general inpatient, acute care, ED, and ICU settings. In addition, a virtual ICU needs to incorporate salient information displays, data analytics, context sensitive checklists and notifications (“smart checklists” and “smart notifications”), as well as reporting features to help clinicians track quality metrics in real time utilizing a single, integrated clinical decision support system with high validity.

There are multitudes of statistics and studies that illustrate an immediate need for remote patient monitoring and virtual ICU’s; In fact two different studies prove hospitals with a dedicated intensivist on staff had a significant reduction in ICU mortality and average length of stay (LOS).²³ Knowing that intensivists have a positive effect on mortality and LOS reductions there are a number of facts to consider. There are 6,000 ICUs but only 5,500 board-certified intensivists.⁴ Even more alarming, in study from 2019 the Society of Critical Care Medicine and Wolters Kluwer stated, “of the 2,814 acute care hospitals studied, 1,469 (52%) had intensivists and 1,345 (48%) had no intensivists”.⁵ As of 2010, less than 15 percent of intensive care units (ICUs) are able to provide intensivist care.⁶ Additionally, “more than 5 million patients are admitted annually to U.S. ICUs for intensive or invasive monitoring; support of airway, breathing, or circulation; stabilization of acute or life-threatening medical problems; comprehensive management of injury and/or illness...ICU patients...all share the need for frequent assessment and a greater need for technological support than patients admitted to non-ICU beds.”⁷
These statistics and studies illustrate a clear need for clinical command centers and remote patient monitoring, especially in the ICU setting. A virtual ICU with remote patient monitoring capable of providing alerts for patient decompensation, abnormal lab results, and the ability to order diagnostics, treatments, procedures, etc. enables critical care teams to have the efficiency to monitor numerous patients across multiple locations. As a result, virtual ICU’s hold the potential and capability to improve the quality of care delivered in critical care environments while increasing the throughput of intensivists. Ambient Clinical Analytics remote patient monitoring and virtual ICU enterprise class products are designed to fit a hospitals Lean Quality & Six Sigma in Healthcare Programs. Below are some of the high-level benefits of a solution that should be minimal requirements for any hospital or health system considering a virtual ICU model.
Traditional telehealth and virtual ICU have surged across the country in the wake of COVID-19, but traditional telehealth solutions only solve a portion of the problem. Virtual-ICU software requires FDA clearance for active patient monitoring. Access to traditional telehealth, integrated with additional clinical analytics and data visualization, presents a complete platform for a Virtual ICU. Integrated virtual ICU platforms help physicians and nurses effectively monitor all hospital beds, in addition to the ICU beds, and will help track patient deterioration using automatic APACHE IV, SOFA, Sepsis, & Ventilator Induced Lung Injury (VILI) types of scoring and sniffers. Integrating early warnings and changes in patient condition with traditional telehealth software, along with the ability to track patients from admit to discharge, make virtual ICU platforms ideal for dealing with the current intensivist shortage.
The complexity of today’s ICU services entails the need for sharing health information through off-site ICU centers.⁹ Virtual ICU platforms drive situational awareness through real-time point of care access to vital process-of-care information and real time analytics, allowing providers to remotely monitor and manage every bed in the health system like it is an ICU bed. Remote Patient Monitoring and Virtual ICU’s, extended to all beds in a hospital, increase a health systems ability to handle ICU surge and improves the safety for both the clinicians and the patients.
Summary
It is evident that despite improvements in modern tele-ICU’s, most current approaches to virtual ICU care and remote patient monitoring fall short of providing the data visualization and clinical decision support tools required to effectively care for critically ill patients. Over the years and especially through this pandemic, we have learned that AWARE's innovative virtual ICU UX design focuses on delivering those requirements while reducing information overload and making it possible to prioritize clinically important information. AWARE’s Remote Patient Monitoring implementations have been associated with marked improvement in clinical outcomes. Adjusted for illness severity, the odds for hospital mortality of critically ill patients treated after AWARE implementation were reduced by half (odds ratio 0.45, 95% confidence interval 0.30 to 0.70). In addition, the length of ICU stay decreased by 50%, length of hospital stays by 37%, and total charges for hospital stay by 30% ($43,745 per hospital admission).¹⁰ Other key outcomes that have been measured include:
AWARE™ Critical Care
Ambient has achieved FDA Class II Clearance, CE Marking, and ISO 13485:2016 Certification on the AWARE™ platform. AWARE™ provides remote patient monitoring and predictive analytics combined with novel clinical decision support tools, decreases provider fatigue, reduces errors, and saves lives. Created by clinicians for clinicians, AWARE™ delivers real-time virtual ICU surveillance, situational awareness, and actionable information to the care team, improving outcomes and reducing costs in critical care and general inpatient areas.

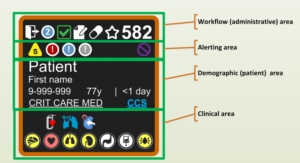
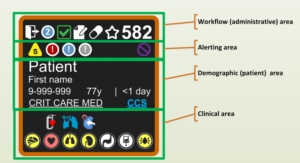
AWARE’s (Ambient Warning and Response Evaluation) virtual ICU solution is designed to provide bedside and remote patient monitoring using data visualization and clinical analytics. The AWARE™ Multi-Patient Viewer (MPV) and Single-Patient Viewer (SPV) allows all nurses and physicians to view a patient through the eyes of a intensivists. Critical care requires turning massive amounts of raw data into actionable knowledge and many of the electronic tools at your disposal make this much more complicated than necessary.
This complication, commonly known as information overload, frustrates clinicians and exposes patients to diagnostic errors and therapeutic harm. AWARE™ is different, it was built by intensivists at Mayo Clinic using principles of human factors engineering, gathering the data that’s important to critical care teams and displaying it in a way that minimizes cognitive load. AWARE™ is the gold standard for how smart clinical analytics and data visualization can improve communication, efficiency, situational awareness, and safety. Unlike any other system, AWARE™ shows you what you need to see, at the point of care and in virtual ICU settings, organized the way an intensivist approaches their patients’ data.
AWARE Clinical Control Tower™ is a solution designed to provide a virtual ICU for AWARE™ Critical Care and Sepsis DART™ with centralized remote patient monitoring and collaboration for physicians and nurses. AWARE™ and Sepsis DART™ capabilities are delivered to all locations in a standardized format, eliminating EMR differences. Clinical Control Tower™ provides distributed tele-health, virtual ICU and remote patient monitoring within your system and with contracted facilities.

Whether deployed in an ICU or as a virtual ICU solution, the AWARE™ enterprise class family of solutions including Sepsis DART, AWARE Critical Care, and Clinical Control Tower all help you approach your patients in a more effective, informed, and organized fashion while decreasing provider fatigue, reducing errors, and saving lives. Created by clinicians for clinicians, AWARE™ delivers real-time surveillance, situational awareness, and actionable information to the care team, improving outcomes and reducing costs in critical care and general inpatient areas.
The combination of effective predictive analytics and advanced clinical decision support tools helps to reduces errors, improve patient outcomes, reduce the cost of care, and deliver best-care practices for ICUs and other inpatient care areas. AWARE’s predictive analytics system provides a “smart view” via data visualization of Electronic Health Record data that reduces the risk of medical errors and improves patient outcomes with high reliability healthcare. It works with your EMR and bedside monitors to present only relevant information for care delivery. This minimizes information overload, which is a leading cause of medical errors, and results in a lower cost of care. By facilitating quick access to patients’ information at the point of care and in remote patient monitoring centers using AWARE’s Clinical Control Tower™, Ambient aids interventional decision-making and is proven to reduce the incidence of cognitive errors by 50%.

For more detailed information on Ambient Clinical Analytics and Virtual ICU or Remote Patient Monitoring solutions for your hospital or health system, or for our published studies on AWARE™ please contact tim.kuebelbeck@ambientclinical.com.
About Ambient Clinical Analytics - As an industry leader, Ambient is supporting leading healthcare systems and has done so since its founding in 2013. Our solutions are designed by clinicians to be easy-to-use by every caregiver in your organization and are configured to be up and running rapidly. We are trusted by a community of high-performing healthcare providers across the United States. Our solutions are powerful real-time point-of-care and remote healthcare platforms designed to deliver life-saving solutions using data visualization, communication, and analytics based clinical decision support.
Ambient’s AWARE™, Clinical Control Tower™, and Sepsis DART™ solutions are exceptionally secure, high-performance, FDA Class II approved and CE Marking certified Software as a Medical Device (SaMD) platforms designed for remote patient monitoring and virtual ICU’s. Ambient’s Sepsis DART™ product has been accepted into the Patient Safety Movement’s Actionable Patient Safety Solutions (APSS) #9 for Sepsis. Ambient has achieved ISO 13485:2016 certification, an internationally recognized quality standard specific to the medical device industry. The ISO 13485 standard sets out the requirements for a quality management system specific to the medical device industry. Ambient is also deploying the AWARE™ family of solutions, to help manage COVID-19. Ambient’s Virtual ICU and Remote Patient Monitoring platforms are ideal for dealing with current and possible future outbreaks and intensivists staffing deficits. For more information, please visit https://ambientclinical.com.
Citations
As we slowly emerge from the COVID pandemic our goal is simple; help doctors, nurses, hospitals, and health systems solve clinical issues using innovative technology and best practices for Remote Patient Monitoring and the Virtual ICU. The pandemic has been a defining event in many ways for remote patient monitoring and virtual ICU’s. There is a shortage of intensivists in the United States, and the demand for them is increasing with our aging population.¹ At Ambient Clinical Analytics we have learned that a virtual ICU and remote patient monitoring with a smart data visualization approach and innovative technology helps save lives and reduces costs. This blog is to help you understand the importance of remote patient monitoring and virtual ICU’s and why every hospital and health system should either be evaluating, deploying, or already utilizing a novel solution.
Virtual ICU intensivists and nurses providing services to multiple care centers, regardless of their location, is an enormous care advantage for hospitals that don’t have any or adequate intensivists or are not located in a major metropolitan area. A virtual ICU, often at an off-site location, connects critical care teams (both intensivists and nurses) with local caregivers, patients, and families for the purpose of caring for patients located in a hospital setting using audio, video, and clinical decision support tools. Remote intensivists and nurses require the same access to patient data as those who are practicing at the bedside. Many of today’s virtual ICU settings have access to excellent audio and visual tools but are lacking the clinical decision support and smart data visualization tools needed to provide the best care possible for ICU patients. One important point to consider as you read this article is that many virtual ICU solutions were designed for critical care only and are not malleable to general inpatient beds.
Using novel remote patient monitoring solutions such as Ambient Clinical Analytics AWARE™ Critical Care, along with audio and visual virtual ICU solutions, provides alerting for issues like sepsis, heart failure, and patient decompensation that increases efficiency and improves clinical outcomes. Disruptive virtual ICU solutions must also monitor other changes in patient status including medication changes, abnormal labs, etc. Any virtual ICU solution you choose must promote situational awareness for patients in all hospital locations, including general inpatient, acute care, ED, and ICU settings. In addition, a virtual ICU needs to incorporate salient information displays, data analytics, context sensitive checklists and notifications (“smart checklists” and “smart notifications”), as well as reporting features to help clinicians track quality metrics in real time utilizing a single, integrated clinical decision support system with high validity.

There are multitudes of statistics and studies that illustrate an immediate need for remote patient monitoring and virtual ICU’s; In fact two different studies prove hospitals with a dedicated intensivist on staff had a significant reduction in ICU mortality and average length of stay (LOS).²³ Knowing that intensivists have a positive effect on mortality and LOS reductions there are a number of facts to consider. There are 6,000 ICUs but only 5,500 board-certified intensivists.⁴ Even more alarming, in study from 2019 the Society of Critical Care Medicine and Wolters Kluwer stated, “of the 2,814 acute care hospitals studied, 1,469 (52%) had intensivists and 1,345 (48%) had no intensivists”.⁵ As of 2010, less than 15 percent of intensive care units (ICUs) are able to provide intensivist care.⁶ Additionally, “more than 5 million patients are admitted annually to U.S. ICUs for intensive or invasive monitoring; support of airway, breathing, or circulation; stabilization of acute or life-threatening medical problems; comprehensive management of injury and/or illness...ICU patients...all share the need for frequent assessment and a greater need for technological support than patients admitted to non-ICU beds.”⁷
These statistics and studies illustrate a clear need for clinical command centers and remote patient monitoring, especially in the ICU setting. A virtual ICU with remote patient monitoring capable of providing alerts for patient decompensation, abnormal lab results, and the ability to order diagnostics, treatments, procedures, etc. enables critical care teams to have the efficiency to monitor numerous patients across multiple locations. As a result, virtual ICU’s hold the potential and capability to improve the quality of care delivered in critical care environments while increasing the throughput of intensivists. Ambient Clinical Analytics remote patient monitoring and virtual ICU enterprise class products are designed to fit a hospitals Lean Quality & Six Sigma in Healthcare Programs. Below are some of the high-level benefits of a solution that should be minimal requirements for any hospital or health system considering a virtual ICU model.
- Proven to reduce errors and improve efficiency (as demonstrated in Mayo Clinic published research)⁸
- Products align with all key lean six sigma / quality tools to support a hospital’s improvement projects
- Easy to install with minimal hospital IT support required
- Intuitive/User friendly UX design that requires little or no training to start using the products
- Reasonable subscription-based pricing that demonstrates an ROI within several months
- Facilitates ‘Lean Six Sigma Healthcare Quality’ initiatives in health systems and hospitals

Traditional telehealth and virtual ICU have surged across the country in the wake of COVID-19, but traditional telehealth solutions only solve a portion of the problem. Virtual-ICU software requires FDA clearance for active patient monitoring. Access to traditional telehealth, integrated with additional clinical analytics and data visualization, presents a complete platform for a Virtual ICU. Integrated virtual ICU platforms help physicians and nurses effectively monitor all hospital beds, in addition to the ICU beds, and will help track patient deterioration using automatic APACHE IV, SOFA, Sepsis, & Ventilator Induced Lung Injury (VILI) types of scoring and sniffers. Integrating early warnings and changes in patient condition with traditional telehealth software, along with the ability to track patients from admit to discharge, make virtual ICU platforms ideal for dealing with the current intensivist shortage.
The complexity of today’s ICU services entails the need for sharing health information through off-site ICU centers.⁹ Virtual ICU platforms drive situational awareness through real-time point of care access to vital process-of-care information and real time analytics, allowing providers to remotely monitor and manage every bed in the health system like it is an ICU bed. Remote Patient Monitoring and Virtual ICU’s, extended to all beds in a hospital, increase a health systems ability to handle ICU surge and improves the safety for both the clinicians and the patients.
Summary
It is evident that despite improvements in modern tele-ICU’s, most current approaches to virtual ICU care and remote patient monitoring fall short of providing the data visualization and clinical decision support tools required to effectively care for critically ill patients. Over the years and especially through this pandemic, we have learned that AWARE's innovative virtual ICU UX design focuses on delivering those requirements while reducing information overload and making it possible to prioritize clinically important information. AWARE’s Remote Patient Monitoring implementations have been associated with marked improvement in clinical outcomes. Adjusted for illness severity, the odds for hospital mortality of critically ill patients treated after AWARE implementation were reduced by half (odds ratio 0.45, 95% confidence interval 0.30 to 0.70). In addition, the length of ICU stay decreased by 50%, length of hospital stays by 37%, and total charges for hospital stay by 30% ($43,745 per hospital admission).¹⁰ Other key outcomes that have been measured include:
- Provider Level: cognitive load, safety culture, team communication, satisfaction, technology usage.
- System Level: Processes of care targets will be identified with local practice but may include items such as use of non-invasive and low tidal volume modes of ventilation, judicious fluid resuscitation and shock reversal, restricted blood product use, DVT prophylaxis, central device removal, goals of care discussion, and sepsis bundle of care compliance.
- Patient Level: ICU and overall hospital mortality (unadjusted and severity of illness adjusted), ICU and overall hospital length of stay, ventilator free days, discharge location, and better communications to families.
- Unit Level: Development of numerous unit-based algorithms covering all aspects of critical care.
AWARE™ Critical Care
Ambient has achieved FDA Class II Clearance, CE Marking, and ISO 13485:2016 Certification on the AWARE™ platform. AWARE™ provides remote patient monitoring and predictive analytics combined with novel clinical decision support tools, decreases provider fatigue, reduces errors, and saves lives. Created by clinicians for clinicians, AWARE™ delivers real-time virtual ICU surveillance, situational awareness, and actionable information to the care team, improving outcomes and reducing costs in critical care and general inpatient areas.

AWARE’s (Ambient Warning and Response Evaluation) virtual ICU solution is designed to provide bedside and remote patient monitoring using data visualization and clinical analytics. The AWARE™ Multi-Patient Viewer (MPV) and Single-Patient Viewer (SPV) allows all nurses and physicians to view a patient through the eyes of a intensivists. Critical care requires turning massive amounts of raw data into actionable knowledge and many of the electronic tools at your disposal make this much more complicated than necessary.
This complication, commonly known as information overload, frustrates clinicians and exposes patients to diagnostic errors and therapeutic harm. AWARE™ is different, it was built by intensivists at Mayo Clinic using principles of human factors engineering, gathering the data that’s important to critical care teams and displaying it in a way that minimizes cognitive load. AWARE™ is the gold standard for how smart clinical analytics and data visualization can improve communication, efficiency, situational awareness, and safety. Unlike any other system, AWARE™ shows you what you need to see, at the point of care and in virtual ICU settings, organized the way an intensivist approaches their patients’ data.
AWARE Clinical Control Tower™ is a solution designed to provide a virtual ICU for AWARE™ Critical Care and Sepsis DART™ with centralized remote patient monitoring and collaboration for physicians and nurses. AWARE™ and Sepsis DART™ capabilities are delivered to all locations in a standardized format, eliminating EMR differences. Clinical Control Tower™ provides distributed tele-health, virtual ICU and remote patient monitoring within your system and with contracted facilities.

Whether deployed in an ICU or as a virtual ICU solution, the AWARE™ enterprise class family of solutions including Sepsis DART, AWARE Critical Care, and Clinical Control Tower all help you approach your patients in a more effective, informed, and organized fashion while decreasing provider fatigue, reducing errors, and saving lives. Created by clinicians for clinicians, AWARE™ delivers real-time surveillance, situational awareness, and actionable information to the care team, improving outcomes and reducing costs in critical care and general inpatient areas.
The combination of effective predictive analytics and advanced clinical decision support tools helps to reduces errors, improve patient outcomes, reduce the cost of care, and deliver best-care practices for ICUs and other inpatient care areas. AWARE’s predictive analytics system provides a “smart view” via data visualization of Electronic Health Record data that reduces the risk of medical errors and improves patient outcomes with high reliability healthcare. It works with your EMR and bedside monitors to present only relevant information for care delivery. This minimizes information overload, which is a leading cause of medical errors, and results in a lower cost of care. By facilitating quick access to patients’ information at the point of care and in remote patient monitoring centers using AWARE’s Clinical Control Tower™, Ambient aids interventional decision-making and is proven to reduce the incidence of cognitive errors by 50%.

For more detailed information on Ambient Clinical Analytics and Virtual ICU or Remote Patient Monitoring solutions for your hospital or health system, or for our published studies on AWARE™ please contact tim.kuebelbeck@ambientclinical.com.
About Ambient Clinical Analytics - As an industry leader, Ambient is supporting leading healthcare systems and has done so since its founding in 2013. Our solutions are designed by clinicians to be easy-to-use by every caregiver in your organization and are configured to be up and running rapidly. We are trusted by a community of high-performing healthcare providers across the United States. Our solutions are powerful real-time point-of-care and remote healthcare platforms designed to deliver life-saving solutions using data visualization, communication, and analytics based clinical decision support.
Ambient’s AWARE™, Clinical Control Tower™, and Sepsis DART™ solutions are exceptionally secure, high-performance, FDA Class II approved and CE Marking certified Software as a Medical Device (SaMD) platforms designed for remote patient monitoring and virtual ICU’s. Ambient’s Sepsis DART™ product has been accepted into the Patient Safety Movement’s Actionable Patient Safety Solutions (APSS) #9 for Sepsis. Ambient has achieved ISO 13485:2016 certification, an internationally recognized quality standard specific to the medical device industry. The ISO 13485 standard sets out the requirements for a quality management system specific to the medical device industry. Ambient is also deploying the AWARE™ family of solutions, to help manage COVID-19. Ambient’s Virtual ICU and Remote Patient Monitoring platforms are ideal for dealing with current and possible future outbreaks and intensivists staffing deficits. For more information, please visit https://ambientclinical.com.
Citations
- Mullen-Fortino, M., J. DiMartino, L. Entrikin, S. Muliner, C. W. Hanson, and J. M. Kahn. “Bedside Nurses’ Perceptions of Intensive Care Unit Telemedicine.” American Journal of Critical Care 21, no. 1 (2012): 24–32.
- Celi, L. A., E. Hassan, C. Marquardt, M. Breslow, and B. Rosenfeld. “The eICU: It’s Not Just Telemedicine.” Critical Care Medicine 29, no 8 (2001): N183–N189.
- Morrison, J. L., Q. Cai, N. Davis, Y. Yan, M. L. Berbaum, M. Ries, and G. Solomon. “Clinical and Economic Outcomes of the Electronic Intensive Care Unit: Results from Two Community Hospitals.” Critical Care Medicine 38, no. 1 (2010): 2–8.
- Ries, M. “Tele-ICU: A New Paradigm in Critical Care.” International Anesthesiology Clinics 47, no. 1 (2009): 153–70.
- https://journals.lww.com/ccmjournal/Abstract/2019/04000/Intensivists_in_U_S__Acute_Care_Hospitals_.4.aspx
- Goran, S. “A Second Set of Eyes: An Introduction to Tele-ICU.” Critical Care Nurse 30, no. 4 (2010): 46–54.
- Society of Critical Care Medicine
- Natalia Olchanski & Mikhail A. Dziadzko & Ing C. Tiong & Craig E. Daniels &Steve G. Peters & John C. O’Horo & Michelle N. Gong, “Can a Novel ICU Data Display Positively Affect Patient Outcomes and Save Lives?” August 29, 2017
- Halpern, N. A., S. M. Pastores, and R. J. Greenstein. “Critical Care Medicine in the United States 1985–2000: An Analysis of Bed Numbers, Use, and Costs.” Critical Care Medicine 32, no. 6 (2004): 1254–59.
- Olchanski, N., et al., Can a Novel ICU Data Display Positively Affect Patient Outcomes and Save Lives? J Med Syst, 2017. 41(11): p. 171.

